Foot blisters are considered one of the most common injuries in sport. Blister incidence has been investigated in athletes, hikers and military populations and ranges from 33% - 50% (Brennan et al, 2012; Richie, 2010). And research has shown that there is a large range of individual susceptibility to blister formation (Hashmi et al, 2013; Sulzberger et al, 1966; Yavuz and Davis, 2010).
In fact, blisters are probably one of the more common injuries in everyday life. Although painful, blisters are so familiar that they’re often ‘beneath our notice’ and not taken very seriously. And because the success of preventative methods ranges from mixed to poor, blister treatment becomes the focus.
Podiatrists are of course at the front line of foot blister prevention. But blister prevention tends to be a hit and miss affair. Sometimes it’s as easy as zinc oxide tape, fixomul, or a prophylactic Compeed dressing. Other times it’s a small change to an orthotic prescription or pressure deflection. And sometimes nothing seems to work.
“Partial blister prevention success was certainly my own personal experience. Being a podiatrist, that was quite frustrating, not to mention embarrassing! A few years ago I tried ENGO Blister Prevention Patches. I’ve had great personal success with them and have since become their Australasian distributor. I was impressed yet puzzled by how this product stopped my blisters so well and how it works at the shoe surface rather than on the skin. This led me to investigate the whole topic of foot blisters – to see where this and the other preventative methods fit in.”
Although blisters are common, there are a couple of assumptions and misconceptions about blister causation in the popular media, among sports medicine practitioners and in the medical literature. And there are issues around terminology that cloud a thorough understanding (Carlson, 2001; National Pressure Ulcer Advisory Panel, 2012). A discussion was recently held at Podiatry Arena that highlights some of these issues (“Blisters and Taping” thread).
Friction and rubbing
Most of us would say that blisters are caused by friction; and that friction is rubbing. But that’s not accurate. Friction is not rubbing. Friction is the force that resists the movement of one surface against another; whereas rubbing is the movement of one surface against another. So in fact they are quite the opposite of each other.
The causative mechanism of blisters is the shear that occurs before rubbing. This concept is represented for the back of the heel in this video loop. Shear reaches its peak just before the rub starts (Carlson, 2006; Carlson, 2011; Yavus & Davis, 2010).
Figure 1 (video): High friction levels between the shoe (orange), sock (white) and skin (brown) keep these 3 surfaces stuck to each other. Yet inside the foot, the calcaneus bone moves up and down. The purple section represents a section of soft tissue at the back of the heel. As the bone moves up, this section of soft tissue stretches (shears). This is what causes blisters.
Shear is the parallel stretching and distortion of tissue layers across one another. As one of the influencing factors to shear, friction is a big part of the foot blister story. The measurement of friction is the coefficient of friction (COF). The COF is a number usually below 1.0 and represents the level of friction between two surfaces. In the literature around blisters, the standard material against which a material’s COF is calculated is cotton (cotton sock/stockinette). The COF of most materials in the in-shoe environment is between 0.4 – 0.9. (Carlson, 2001; Payette, 2010; Sanders et al, 1998).
Interfaces and friction
When wearing shoes and socks, there are two material interfaces: the shoe-sock interface and the skin-sock interface. The moist in-shoe environment during exercise sees a high COF at both interfaces. This high friction force causes the skin, sock and shoe to remain in stationary contact. Meanwhile, the bones are moving back and forth. The resultant shear can lead to blisters. The higher the friction and the larger the skeletal movement, the larger the shear distortion and likelihood of blister formation. The zone of least resistance to shear is the stratum spinosum of the epidermis. Blisters are more common on the feet (particularly the plantar surface) because of the thicker outer stratum corneum (Naylor, 1955) and because the skin is adhered more firmly to underlying structures (Akers, 1972; Akers, 1977; Carlson, 2011).
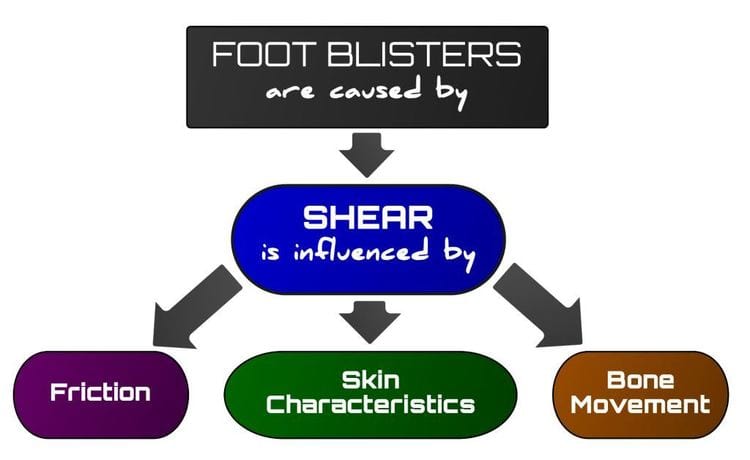
Figure 2: Blisters are an injury of shear. Shear is influenced by friction, skin characteristics and the amount of relative bony movement.
The feet can deal with a lot of shear without adverse effect, particularly if given time to adapt to the shoes / activity / terrain. It’s only when shear is excessive and/or repetitive that blisters will develop.
To stop blisters from forming, shear peaks can be lowered either by:
- Reducing the COF at one of the interfaces, allowing a small and early glide at that interface
- Reducing the relative bony excursion
One must remember that in-shoe friction is necessary for effective gait. Friction provides the traction required for propulsion, deceleration and changes of direction during gait. In itself, friction is not bad and the aim of blister prevention should not be to reduce friction globally.
Friction and heat
It is universally stated that heat causes blisters. This leads people to assume that it’s the rubbing against the skin that causes localised over-heating resulting in a burn; much like how two sticks rubbed together can start a fire. But although rubbing increases local skin surface temperature, the maximum temperatures found of around 44 degrees Celsius are insufficient to cause thermal burns. And thermal burn blisters are second degree burns. By definition, a second degree burn occurs to the level of the dermis. In contrast, ‘friction’ blisters occur only as deep as the stratum spinosum of the epidermis.
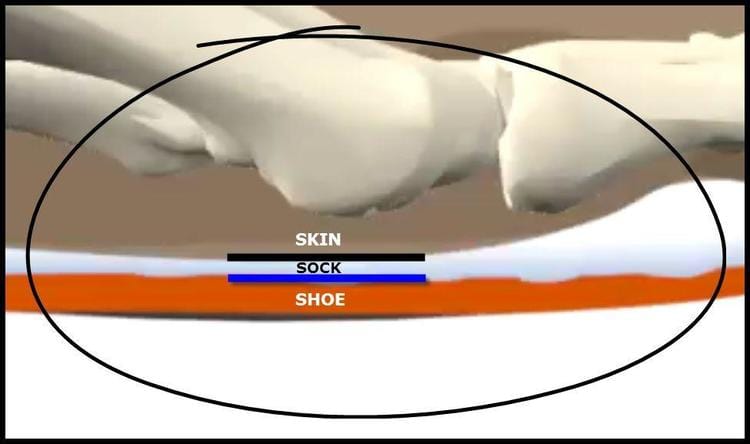
Figure 3: There are two material interfaces that are relevant to the blister formation scenario: the shoe-sock interface and the skin-sock interface.
It is true that burns can cause blisters. But foot “friction” blisters are not thermal burns:
- There is evidence that shows blister incidence is higher in warmer temperatures and lower in colder temperatures (Akers, 1977). But is the increased skin temperature the primary reason for the blister? Or does the increased temperature lead to increased perspiration which increases the in-shoe friction coefficients and therefore increased blister incidence? The latter is certainly true (Nacht et al, 1981; Naylor, 1955). The former has little research to support it and seems to be more of an assumption made.
- Although rubbing increases local skin surface temperature, the maximum temperatures found of around 44 degrees Celsius are insufficient to cause thermal burns (Comaish, 1973; Hashmi, 2013).
- Thermal burn blisters are second degree burns (http://en.wikipedia.org/wiki/Burn). By definition, a second degree burn occurs to the level of the dermis. In contrast, ‘friction’ blisters occur only as deep as the stratum spinosum of the epidermis (Knapik, 1995).
A structured approach to blister prevention
The flowchart below shows there are many areas for practitioners to have a preventative impact on foot blisters. While there is probably not much that is new here to Podiatrists, what is new is the framework. The framework is built from an accurate understanding of blister causative mechanisms and influencing factors. With this, a logical and structured approach to blister prevention can be taken by practitioners – in the therapeutic intervention provided and advice given.
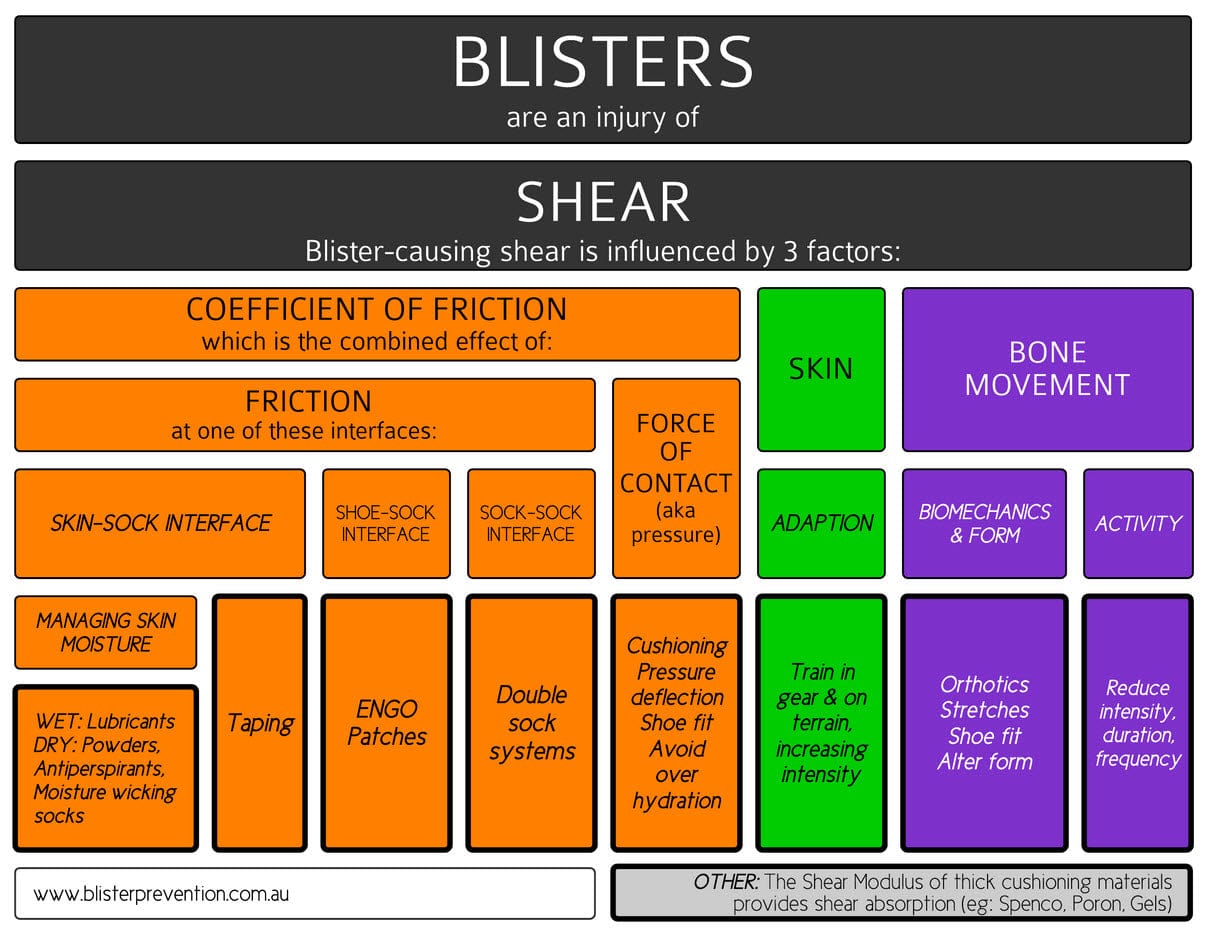
Figure 4: A framework outlining the influencing factors of foot blisters and the preventative interventions that stem from each
Conclusion
Foot blisters deserve more attention and improved outcomes considering their prevalence. It’s not that blisters are an insignificant injury – just take Andy Murray’s 2013 Australian Open final situation as an example. But it seems that because they are an injury of the skin rather than the musculoskeletal system, they tend to be relegated to an injury of lesser importance. Practitioners involved in foot blister management should have an accurate understanding of blister causation to help them identify where preventative opportunities exist.
References
- Akers, WA. 1977. Sulzberger on Friction Blistering. International Journal of Dermatology. 16: 369-72.
- Brennan, FH, Jackson, CR, Olsen, C and Wilson, C. 2012. Blisters on the battlefield: the prevalence of and factors associated with foot friction blisters during operation Iraqi freedom. Military Medicine. 177 (2): 157-162.
- Carlson, JM. 2001. The friction factor. OrthoKinetic Review. 1.7 Nov-Dec, p 1-3.
- Carlson, JM. 2006. Functional limitations from pain caused by repetitive loading on the skin: A review and discussion for practitioners, with new data for limiting friction loads. American Academy of Orthotists & Prosthetists. 18 (4): 93-103.
- Carlson JM. 2011. The mechanics of soft tissue damage: removing the “teeth” from the “rub”. The Academy Today. 7.1 (Feb 2011): A5-7.
- Comaish, JS. 1973. Epidermal Fatigue as a Cause of Friction Blisters. The Lancet. Jan 13: 81-83.
- Hashmi, F, Richards, BS, Forghany, S, Hatton, AL and Nester, CJ. 2013. The Formation of Friction Blisters on the Foot: The Development of a Laboratory-Based Blister Creation Model. Skin Research and Technology. 19: e479-e489.
- Knapik, JJ, Reynolds, K, Duplantis, KL and Jones, BH. 1995. Friction blisters – pathophysiology, prevention and treatment. Sports Medicine. 20 (3): 136-147.
- Nacht, S, Close, J, Yeung, D and Gans, EH. 1981. Skin friction coefficient: changes induced by skin hydration and emollient application and correlation with perceived skin feel. Journal of the Society of Cosmetic Chemists. 32 (March-April): 55-65.
- National Pressure Ulcer Advisory Panel. 2012. Friction Induced Skin Injuries – Are They Pressure Ulcers? A National Pressure Ulcer Advisory Panel White Panel. Nov 20, 2012: 1-3.
- Naylor, P. 1955. Experimental friction blisters. British Journal of Dermatology. 67: 327 – 42.
- Naylor, P. 1955. The skin surface and friction. British Journal of Dermatology. 67: 239 – 48.
- Payette, M. 2010. Friction management for diabetic foot problems. Audiovisual Presentation to the 36th Annual Meeting and Scientific Symposium of the American Academy of Orthotists and Prosthetists. Mark Payette, CO - Friction Management for Diabetic Foot Care
- Podiatry Arena, “Blisters and Taping” thread https://www.podiatry-arena.com/podiatry-forum/showthread.php?t=85834&highlight=blisters&page=1
- Richie, D. 2010. How to manage friction blisters. Podiatry Today. 23 (6): 42-48.
- Sanders, JE, Greve, JM, Mitchell, SB and Zachariah, SG. 1998. Material properties of commonly-used interface materials and their static coefficients of friction with skin and socks. Journal of Rehabilitation Research and Development. 35 (2): 161-176.
- Sulzberger, MB, Cortese, TA, Fishman, L and Wiley, HS. 1966. Studies on blisters produced by friction. The Journal of Investigative Dermatology. 47 (5): 456-465.
- Wikipedia https://en.wikipedia.org/wiki/Burn
- Yavuz, M and Davis, BL. 2010. Plantar shear stress distribution in athletic individuals with frictional foot blisters. Journal of the American Podiatric Medicine Association. 100, (2): 116-120.